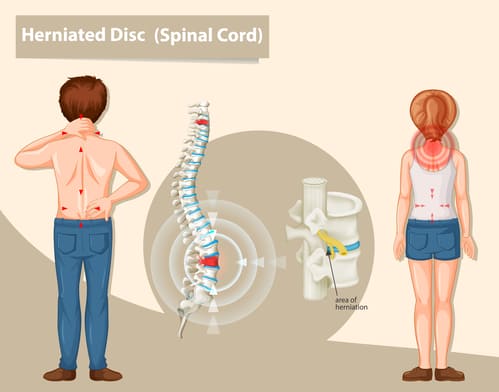
An endoscopic discectomy (ED) is a surgical procedure that is used to remove herniated disc material in the spine. This procedure is minimally invasive and is one of the least invasive surgical techniques available for treating spinal disc herniation.
The procedure is carried out by using a tubular retractor, which is inserted into the body through small incisions. This specialized tube allows the surgeon to observe the spine while minimizing damage to surrounding muscles, which are gently moved to the side and held in place. The doctor administers local anesthesia to ensure patient comfort. With a camera in place, the housing tube serves as a passageway for other surgical instruments used during the ED. The surgeon uses X-ray fluoroscopy for guidance and live visualization and removes the affected discs using a grasper. The tube is then removed, and the small incisions are closed.
The procedure typically takes around 30 minutes and is less traumatic to the spine than traditional open surgeries. Most patients can return home within two to three hours of the procedure.
While there are potential complications associated with any surgery, the risks associated with minimally invasive spinal procedures are significantly lower. In rare cases, nerve damage or persisting pain may occur after the procedure, but these risks can be minimized by communicating any discomfort with your doctor.
Advantages of an Endoscopic Discectomy (ED)
A form of minimally invasive spine surgery, EDs boast the following advantages:
- Minimal blood loss
- Outpatient procedure (no hospitalization required)
- Minimal scar tissue formation due to smaller incisions
- Short recovery time
- High success rate
- Preservation of spinal mobility
- Local anesthesia
- No external stitches

