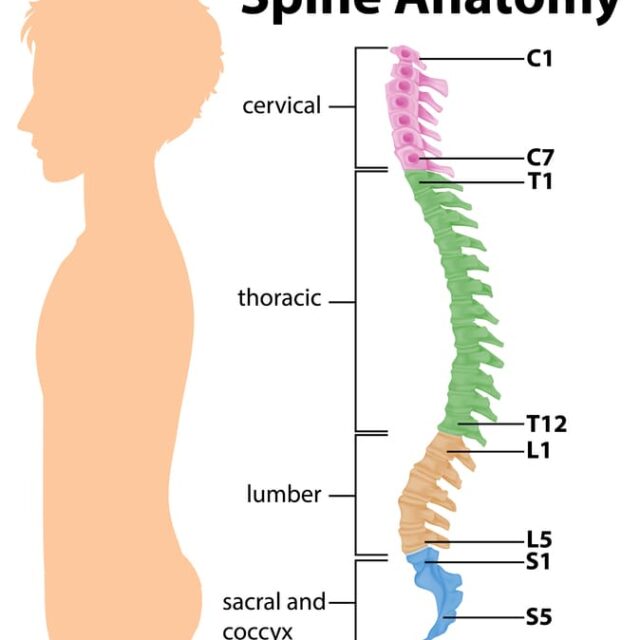
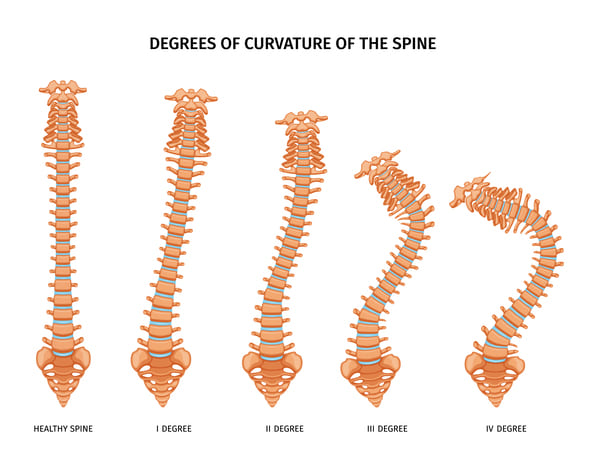
Scoliosis is a condition where the spine curves abnormally, causing it to twist sideways on the coronal plane. Kyphosis, on the other hand, is a sagittal plane deformity where the spine curves forward abnormally, leading to a rounded or hunchback appearance.
The main goals of scoliosis and kyphosis correction surgery are to stop the progression of the curve, reduce deformity, and maintain trunk balance. With the help of modern tools and technology, skilled surgeons trained in deformity correction can achieve safe and effective results. Intra-operative neuromonitoring (IONM) is a technology that allows real-time monitoring of spinal cord function and integrity during scoliosis and kyphosis deformity correction, minimizing the risk of intra-operative spinal cord injury.
For kyphosis, the operation is a spinal fusion. The basic idea is to realign and fuse together the curved vertebrae so that they heal into a single, solid bone.
For scoliosis correction, there are several options, including standard long fusion, growing rod systems, and novel growth-modulating non-fusion (fusionless) anterior vertebral body tethering.

Traditional Posterior Spinal Fusion corrective surgery
It involves permanently fusing two or more adjacent vertebrae so that they grow together at the spinal joint and form a solid bone that no longer moves. Modern surgical approaches and instrumentation—rods, screws, hooks, and/or wires placed in the spine—have enabled spinal fusion surgeries to achieve better curvature correction and faster recovery times than in the past. An advantage of spinal fusion surgery is that it has a long-term record of safety and efficacy for treating scoliosis. While a drawback to the procedure is that any fused vertebrae will lose mobility, which can limit some of the back’s bending and twisting, today’s spinal fusions tend to fuse fewer vertebrae and maintain more mobility than in the past.
Temporary Growing Rod (TGR)
Temporary Growing Rod (TGR) systems aim to delay definitive fusion by utilizing rods anchored to the spine to help correct/maintain the spine’s curvature while the child grows. Every 6 to 12 months, the child has another minor day care procedure to lengthen the rods to keep up with the spine’s growth. Once the child is close enough to skeletal maturity, the child will usually get a definitive spinal fusion. If a spinal fusion is done at too young of an age (typically younger than age 10 in girls or less than 12 in boys), that could leave less room for the lungs to develop, in addition to the child having an unusually short trunk compared to the limbs. To avoid these complications, the growing systems method helps guide the spine as it grows, preventing the curve from worsening as the spine matures and eventually becomes ready for a fusion if needed.
Novel Fusionless (Non-Fusion)
Novel Fusionless (Non-Fusion) Scoliosis Correction Surgery uses the growth modulation ability of the child’s spine, similar to what has been done in the past to treat unequal leg heights in growing children. The theory is that by putting constant pressure on a bone, it will grow slower and denser. By applying such pressure on the outer side of a spinal curve, the surgeon aims to slow or stop the growth of the curve’s outer side while the curve’s inner side continues to grow normally. As the spine continues to grow in this manner, the lateral curvature should reduce, and the spine should become straighter.
Anterior Vertebral Body Tethering (AVBT)
Anterior vertebral body tethering (AVBT) is a fusionless method that uses an AVBT system, which involves placing screws on the outer side of the curve and then tensioning them taut with a cord so the spine straightens. Compared to spinal fusion, fusionless surgery has the potential benefit of retaining more spinal mobility and flexibility and being less invasive than standard posterior corrective spinal fusion procedures. However, this is a newer approach, and long-term data about the risks and benefits are not yet available.Scoliosis is a condition where the spine curves abnormally, causing it to twist sideways on the coronal plane. Kyphosis, on the other hand, is a sagittal plane deformity where the spine curves forward abnormally, leading to a rounded or hunchback appearance.
The main goals of scoliosis and kyphosis correction surgery are to stop the progression of the curve, reduce deformity, and maintain trunk balance. With the help of modern tools and technology, skilled surgeons trained in deformity correction can achieve safe and effective results. Intra-operative neuromonitoring (IONM) is a technology that allows real-time monitoring of spinal cord function and integrity during scoliosis and kyphosis deformity correction, minimizing the risk of intra-operative spinal cord injury.

